Living with diabetes in Cambodia
- stiftungkanthaboph
- Feb 26
- 4 min read
On Monday afternoon, Menglis, a 5-year-old boy, is brought to the pediatric intensive care unit by his father, who is visibly worried about his son's health. Menglis is unconscious, breathing rapidly and deeply, with his abdomen visibly expanding with each breath (a medical condition known as Kussmaul breathing). He is extremely thin and appears dehydrated. His father reports that for about ten days, Menglis has been feeling very tired, urinating much more frequently than usual, and has lost a significant amount of weight.
For the doctors, the most likely diagnosis is clear: the child has Type 1 diabetes and has arrived at the hospital with one of the severe complications that arise when the disease is not managed properly: diabetic ketoacidosis (DKA), a medical emergency that, if not treated correctly, can be fatal.
The nursing team arrives immediately, and within minutes, they take a blood sample to check his blood sugar levels, electrolytes, and pH. He is given an IV to rehydrate him and a urinary catheter to analyze his urine and monitor his output.
Throughout the afternoon, blood tests confirm the diagnosis. Menglis is slowly rehydrated, and insulin is administered to gradually lower his blood sugar. He is closely monitored, with hourly checks of his blood glucose levels, pH, and electrolytes.
When I return the next day, Menglis is breathing normally and has regained consciousness, although he remains very drowsy. His father never leaves his side, staying with him the entire time I am in the room.
After three days, Menglis’s condition has finally stabilized. He is more active and is even able to eat. He is now ready to be transferred to the hospital’s Diabetic Unit, where he will stay for a few more days, usually about a week, to learn how to manage his new condition before he can be discharged.
In the first photo, we can see Menglis with his father, the intensive care medical team, and Professor Chantana. In the second photo, Menglis is at home after being discharged from the hospital.
Menglis’s bed is now empty, but my mind is filled with countless thoughts: How will a young child manage such a demanding disease, especially with a parent who has little education and may not be able to support him at all times? How will his family afford medical expenses, considering the need for frequent blood sugar checks, insulin injections, and regular medical visits?
And Menglis is not the only one facing this situation. In the past 30 years, nearly 700 children in Cambodia have been diagnosed with Type 1 diabetes. Many of them come from extremely poor families who cannot afford the medical costs associated with diabetes and have parents with low levels of education, making it difficult for them to fully understand and manage the disease.
I discuss my concerns with one of the doctors working in intensive care. He suggests that I spend a day in the Diabetic Unit to observe the follow-up care for young diabetic patients and better understand how they are managed.
Type 1 diabetes is a chronic condition that occurs when the body does not produce insulin. Without insulin, glucose cannot enter the cells and remains in the bloodstream instead of being used for energy, leading to serious health problems. For this reason, individuals with Type 1 diabetes must take insulin every day to keep their blood sugar levels stable. If not properly managed in the long term, diabetes can lead to complications caused by excessive sugar in the blood, such as damage to the eyes, kidneys, and nerves, as well as cardiovascular problems. The amount of insulin injected must also be carefully balanced according to food intake and daily physical activity. Otherwise, blood sugar levels can drop too low, leading to symptoms such as weakness, trembling, confusion and, in severe cases, loss of consciousness.
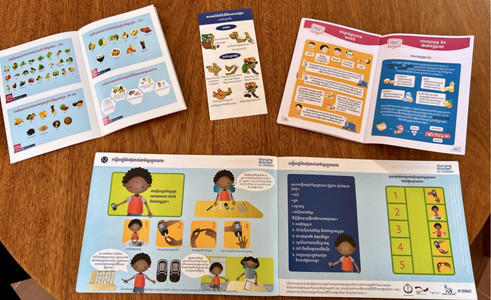
With proper insulin therapy and a balanced diet, Type 1 diabetes can be effectively managed. However, to achieve this, it is essential that patients and their families have the knowledge and tools they need. This includes receiving adequate education about the disease and its management, understanding possible complications, recognizing the symptoms of hypoglycemia, learning how to measure blood sugar, correctly dosing insulin, and following an appropriate diet.
At Kantha Bopha, a dedicated outpatient clinic for diabetic patients is set up every Wednesday. The hospital currently follows approximately 220 children, who must visit the Diabetic Unit every two months for check-ups.
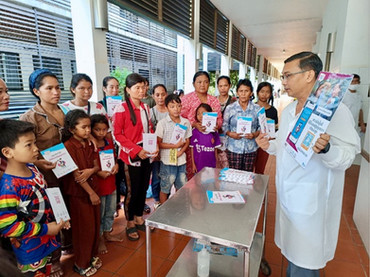
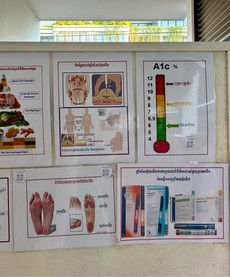
Here, patients and their families receive repeated explanations of key information about diabetes: how to recognize signs of hypoglycemia, administer insulin injections, estimate the sugar content of meals, and much more. To aid comprehension, posters are displayed on the walls, and illustrated booklets with simple explanations in Khmer are distributed.
Picture top right: Dr. Ham Sothea explains a lot about diabetes to the children.
After the training session, it is time to review the blood sugar levels recorded by the patients between check-ups.
Afterward, the hospital provides all the necessary medications and equipment for managing the disease free of charge.
During my visit to the Diabetic Unit, I find answers to all my questions and concerns. Children with diabetes receive careful follow-up care even after being discharged from the hospital, with frequent check-ups where healthcare staff take the time to educate them and reinforce the most important aspects of managing the disease. Additionally, the hospital provides all necessary medications free of charge and covers transportation costs for patients who live far away.
Thanks to Kantha Bopha, Leng was not only saved during the acute phase of his illness but continues to receive care and support at home. I believe this is a great example of how an accessible healthcare system can truly make a difference in the lives of these children.
With best regards from Siem Reap
Laura

















Comentários